Inflammation Research


Siena, Nov 6, 2016
Prof. Ji Zhang Editor, Inflammation ResearchRE: Cortelazzo et al. INRE-D-16-00277 – Revision 1
Dear Editor,
Many thanks to the independent reviewer for insightful review of our Ms titled “Inflammatory protein response in CDKL5-Rett syndrome: evidence of a subclinical smouldering”, by Cortelazzo et al.
We do agree to include two clinical illness scoring scales, before and after ω-3 PUFAs treatment, in order to better clarify the clinical improvement following PUFAs supplementation, and their possible relationships with cytokines/proteins levels. In particular, we added the data of from RCSS [1] and MBAS [2], due to well known illness severity scores scales from Rett syndrome. Results were added to the proper section of the manuscript and their implications briefly discussed, along with possible future directions.
Please find enclosed: i) a brief point-by-point response and ii) the reviewed manuscript with an extra Figure (Figure 2) and two supplementary extra tables (Supplementary Table 3 and 4). Please note that changes to the manuscript were highlighted in red. We look forward to hearing from you in due course Best regards Alessio Cortelazzo
We look forward to hearing from you in due course
Best regards
Alessio Cortelazzo
References
1. Neul JL, et al. Neurology. 2008;70(16):1313-21.
2. FitzGerald PM, et al. Mov Disord. 1990;3(5):195-202.
POINT-BY-POINT RESPONSE
COMMENTS FOR AUTHOR:
This is an interesting study which provided details about immune profile in CDKL5-RTT and MECP2-RTT patients. Data demonstrated characteristics of plasma protein, cytokine levels in both variants. Although whether and how these inflammation related proteins/cytokines contribute to the disease was not fully studied, the authors revealed their regulation following omega3 polyunsaturated fatty acids (ω3 PUFAs) supplementation. I would suggest including the data of clinical examination before and during ω3 PUFAs.
Such data is very useful and will strengthen the study by indicating whether there is a correlation between the level of inflammatory mediators and clinical symptoms (maybe some improvements in some aspects). If the data is not available, at least, a brief discussion on the significance of the study and future direction will be appreciated.
RESPONSE:
We thank the reviewer for favourable comments. We do agree to include two clinical illness
scoring scales, before and after ω-3 PUFAs treatment, in order to better clarify the clinical
improvement following ω-3 PUFAs supplementation, and their possible relationships with
cytokines/proteins levels. In particular, we added the data of from RCSS [1] and MBAS [2], due to well known illness severity scores scales from Rett syndrome.
We included an extra figure (Figure 2, as composed by 5 separate panels in order to be
combined as more convenient for your journal; see below):
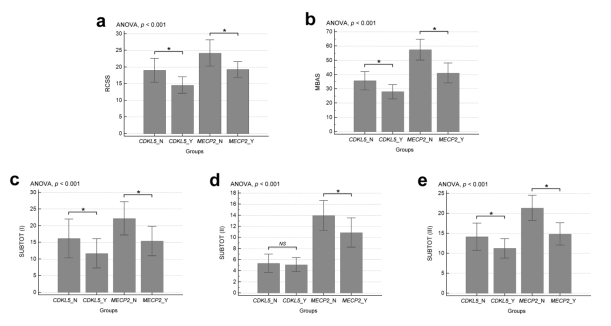
Fig. 2 Clinical illness severity in RTT. The different groups correspond to either CDKL5-RTT or MECP2-RTT,
before (“N” = No) and after (“Y” = Yes) ω-3 PUFAs treatment. Two different scales were evaluated: Rett
syndrome Clinical Severity Scale (RCSS) (a) and Motor-Behavioural Assessment Scale (MBAS) (b) with its
sub-total scorings (“SUBTOT”), I (c), II (d), and III (e). Two-tailed p-value < 0.05 (*); NS, not significant.
We also implemented the Material and Methods section by adding the methodology for
measuring illness severity in RTT. Moreover, we added a short extra paragraph to the Results
section. The corresponding data were briefly discussed (see Discussion section).
In particular, we evaluated the correlations between the level of the inflammatory mediators
and clinical severity (Supplementary Table 3 and 4)
References
1. Neul JL, Fang P, Barrish J, Lane J, Caeg EB, Smith EO, et al. Specific mutations in methyl-CpG-binding
protein 2 confer different severity in Rett syndrome. Neurology. 2008;70(16):1313-21.
2. FitzGerald PM, Jankovic J, Percy AK. Rett syndrome and associated movement disorders. Mov Disord. 1990;3(5):195-202.
Inflammatory protein response in CDKL5-Rett syndrome: evidence of a subclinical smouldering inflammation
Alessio Cortelazzo,
1,2,3,* Claudio De Felice,
4,* Silvia Leoncini,
1,5,* Cinzia Signorini,
5 Roberto
Guerranti,
2,3 Roberto Leoncini,
2,3 Alessandro Armini,
6 Luca Bini,
6 Lucia Ciccoli,
5
and Joussef Hayek1
1 Child Neuropsychiatry Unit, University Hospital Azienda Ospedaliera Universitaria Senese
(AOUS), Viale M. Bracci 16, 53100 Siena, Italy
2 Department of Medical Biotechnologies, University of Siena, Via A. Moro 2, 53100 Siena, Italy
3 Clinical Pathology Laboratory Unit, University Hospital AOUS, Viale M. Bracci 16, 53100 Siena,
Italy
4 Neonatal Intensive Care Unit, University Hospital AOUS, Viale M. Bracci 16, 53100 Siena, Italy
5 Department of Molecular and Developmental Medicine, University of Siena, Via A. Moro 6,
53100 Siena, Italy
6 Department of Life Sciences, University of Siena, Via A. Moro 2, 53100 Siena, Italy
* These authors contributed equally to this work.
To whom correspondence should be addressed at Child Neuropsychiatry Unit, University Hospital,
Azienda Ospedaliera Universitaria Senese (AOUS), Viale M. Bracci 16, 53100 Siena, Italy.
Tel.: +39 0577 234284; Fax: +39 0577 233117; E-mail: alessio.cortelazzo@biologo.onb.it
Abstract
Background Mutations in the cyclin-dependent kinase-like 5 gene cause a clinical variant of Rett
syndrome (CDKL5-RTT). A role for the acute phase response (APR) is emerging in typical RTT
caused by methyl-CpG binding protein 2 gene mutations (MECP2-RTT). No information is to date
available on the inflammatory protein response in CDKL5-RTT. We evaluated, for the first time,
the APR protein response in CDKL5-RTT.
Methods Protein patterns in albumin- and IgG-depleted plasma proteome from CDKL5-RTT
patients were evaluated by two-dimensional gel electrophoresis/mass spectrometry. The resulting
data were related to circulating cytokines and compared to healthy controls or MECP2-RTT
patients. The effects of omega-3 polyunsaturated fatty acids (ω-3 PUFAs) were evaluated.
Results CDKL5-RTT mutations resulted in a subclinical attenuated inflammation, specifically
characterized by an overexpression of the complement component C3 and CD5 antigen-like, both
strictly related to the inflammatory response. Cytokine dysregulation featuring a bulk increase of
anti-inflammatory cytokines, predominantly IL-10, could explain the unchanged erythrocyte
sedimentation rate and atypical features of inflammation in CDKL5-RTT. Omega-3 PUFAs were
able to counterbalance the pro-inflammatory status.
Conclusion For the first time, we revealed a subclinical smouldering inflammation pattern in
CDKL5-RTT consisting in the coexistence of an atypical APR coupled with a dysregulated cytokine
response.
Keywords Rett syndrome; Cyclin-dependent kinase-like 5; Subclinical inflammation; Acute-phase
proteins; Polyunsaturated fatty acids; Cytokine



